
The incidence of ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter spp.) is alarming. And so are the MDR(Multi-drug resistant) cases and PDR(PAN drug-resistant) cases across the globe. In this scenario, phage therapy has shown a positive impact, however, phage therapy has its limitations. As bacteria evolve, so do their defense mechanisms, limiting phage therapy’s application in clinical settings.
Cystic fibrosis is a genetic disorder characterised by thick, sticky mucus in the lungs, pancreas, and other organs, especially with frequent lung infections. Infection with Pseudomonas aeruginosa(PsA) is the common cause of chronic lung disease, as this bacterium thrives in a moist lung atmosphere. Scientists from the Yale School of Medicine identified cystic fibrosis patients who exhibited MDR and PDR Pseudomonas aeruginosa. In this cohort study, 9 cases were chosen that did not respond to standard cystic fibrosis (CF) therapies. All patients had a clinical course complicated by frequent pulmonary exacerbations despite oral, inhaled, and/or intravenous (IV) antibiotics without evidence of clinical benefit.
Procedure implemented
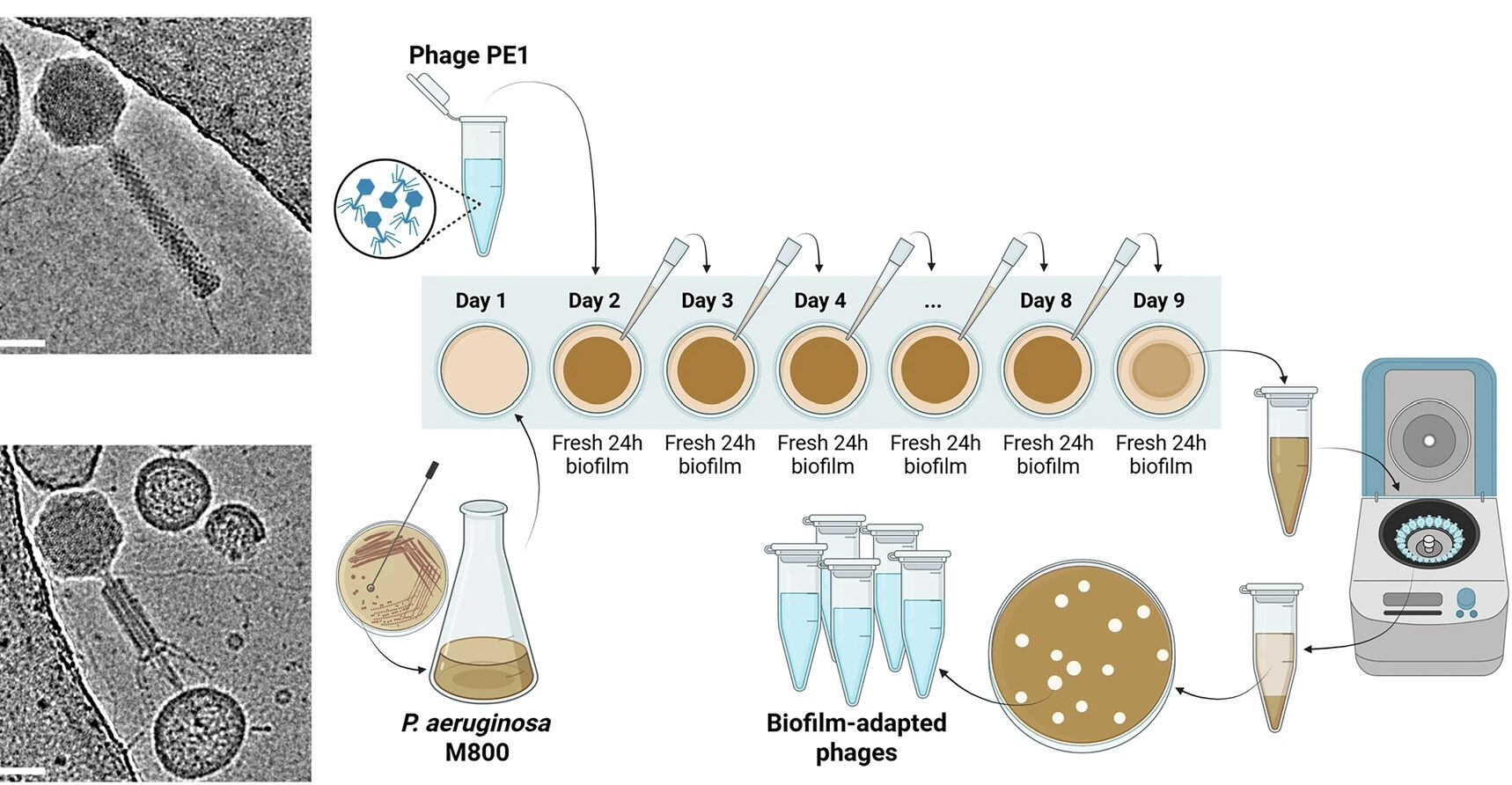
Lytic phages were chosen based on their ability to survive mutants. The study used environmentally sourced phages that were not genetically manipulated. Based on susceptibility testing, phage therapy was framed, and phage isolates were identified from the phage library at Yale’s centre for Phage Biology. These cases were treated on a compassionate basis with personalized phages or a cocktail of phages. Nebulized phage therapy was chosen, instead of IV delivery, to directly target the site of infection and to limit systemic phage exposure, as per the protocol framed. A few days after giving this therapy, their sputum samples were cultured, and the results were astonishing.
The Results
Sputum analysis showed that (1) nebulized phage(s) decreased PsA CFU(Colony Forming Units). (2) Post-phage therapy PsA showed evidence of phage resistance to treatment phages, which suggests that inhaled phages affected PsA in vivo. Researchers also found that the “Sputum P. aeruginosa count has decreased without altering the microbiome”, leading to better lung function among all the participants.
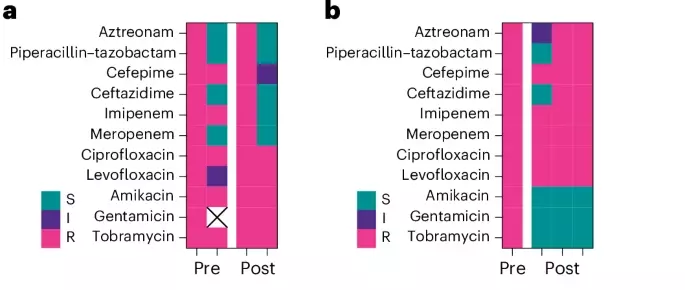
ab Antibiotic susceptibility results from clinical microbiology laboratory testing for sputum isolates taken before and after therapy from patients are shown R resistant S susceptible I intermediate X not reported
P. aeruginosa respiratory infection was found to be a major cause of morbidity and mortality in CF patients. This cohort study promises the ability of inhaled phage therapy to decrease sputum bacteria, especially MDR and PDR pathogens. It proves the potential of phage therapy to translate into promising clinical applications, especially in cystic fibrosis patients
Find the complete article here https://www.nature.com/articles/s41591-025-03678-8

Leave a Reply
You must be logged in to post a comment.