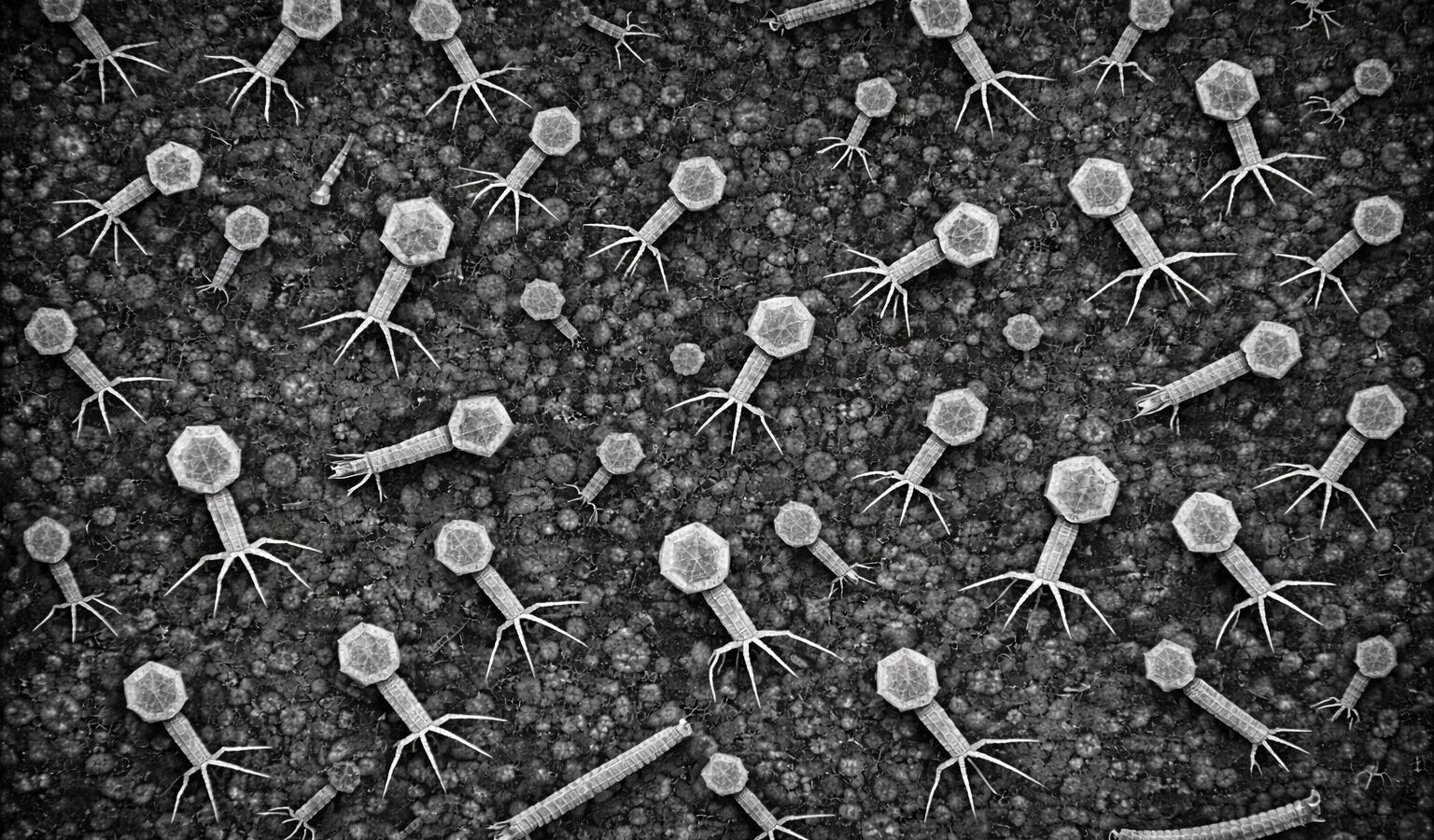
Latest from The Phage
Fresh stories, protocols, and interviews from the phage world.

Phage cocktail cuts fire blight, without disrupting the flower microbiome
Fire blight, caused by Erwinia amylovora, is one of the most destructive bacterial diseases affecting pear and apple orchards. It spreads rapidly…
Is Studying Viromics Worth the Effort?
Many people may not be familiar with the term viromics. Viromics refers to the study of viral communities using metagenomic approaches. Metagenomics,…

Phagebiotics: Are Viruses the Next Gut Health Supplement?
Whenever we think of bacteriophages, we are often faced with very different perspectives on whether they are “good” or “bad.” Interest in…
Phagebiotics: A New Way of Thinking About Gut Health
The idea of phagebiotics comes from a simple shift in how we think about bacteriophages. Instead of viewing them only as tools…
Superinfection exclusion
One of the less talked-about but very interesting roles of bacteriophages is a process known as superinfection exclusion. This happens when a…
How to Succeed in Applying for a Phage-Related PhD (From Someone Who’s Been There)
Applying for a PhD often appears to follow similar expectations across disciplines, particularly the assumption that prior, field-specific experience is essential. However,…