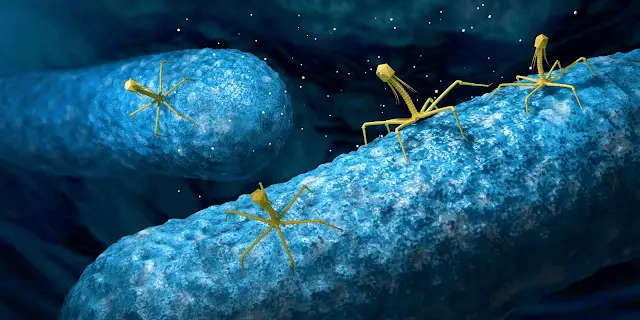
In many countries, antibiotics remain the first-line treatment for bacterial infections, but the rise in antibiotic resistance has led to a decrease in their effectiveness. In some cases, multidrug-resistant strains of bacteria have been successfully treated with bacteriophages. While there is concern about the safety of using phage therapy, there have been very few reports of adverse effects related directly to the therapy.
Despite the success of phage therapy in some cases, there are still challenges to its widespread use. One of the main challenges is the need to identify the specific phages that are effective against a particular bacterial strain, which can be time-consuming and costly. Additionally, regulatory approval for phage therapy is still evolving in many parts of the world, which can limit access to these treatments.
In some scenarios, however, phage therapy may be a preferred option over antibiotics. For example, in cases where antibiotic resistance is a significant concern or where the bacterial infection is caused by a strain that is not susceptible to antibiotics, phage therapy may be a viable treatment option. Additionally, phage therapy may be useful in cases where a personalized treatment approach is needed, such as in chronic infections or infections with multiple bacterial strains.
Why are phages not commonly used in treatments?
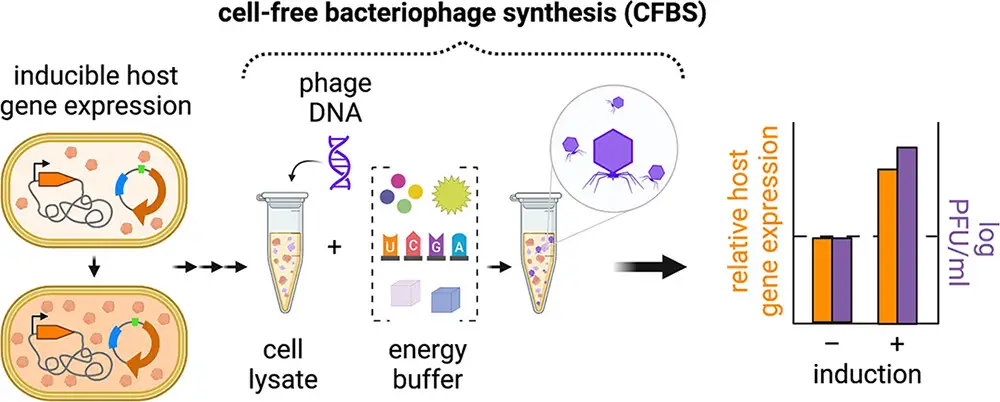
In addition, not all phages are suitable for therapy. Some phages are lysogenic, meaning they integrate their genetic material into the host bacteria’s DNA and do not immediately destroy the bacteria. These types of phages may not be effective for treating infections and can even lead to the transfer of antibiotic resistance genes between bacteria.
Another disadvantage of phage therapy is that it requires a personalized approach. Unlike antibiotics, which can be mass-produced and used to treat a wide range of bacterial infections, phages must be tailored to the specific infection of each patient. This can make phage therapy more expensive and time-consuming than antibiotic treatment.
Finally, the regulatory environment for phage therapy is still evolving in many parts of the world. While phage therapy has a long history of use in countries like Georgia and Poland, it is still considered an experimental treatment in many other countries, including the United States. This can limit access to phage therapy and make it more difficult to develop and distribute phage-based treatments.
Why are antibiotics prevailing despite outstanding phage therapy effectiveness?
Despite the outstanding effectiveness of phage therapy in treating bacterial infections, antibiotics are still the prevailing treatment option in many parts of the world. One of the main reasons for this is the broader host range of antibiotics. Unlike phages, which are typically specific to a particular strain of bacteria, many antibiotics are effective against a wide variety of bacterial species. This makes antibiotics a first-line treatment option for a broad range of bacterial infections.
The development of new antibiotics is also a more established process than the development of phage therapies. Antibiotics are developed through a rigorous process of drug discovery and clinical testing, which is regulated by government agencies such as the FDA in the US. In contrast, the development of phage therapies can be more complex and time-consuming, as it requires the identification of specific phages that are effective against the target bacterial species. Additionally, the regulatory environment for phage therapy is still evolving in many parts of the world, which can limit access to phage therapies.
Despite these challenges, there are still some scenarios in which phage therapy may be preferred over antibiotics. For example, in cases where antibiotic resistance is a significant concern or where the bacterial infection is caused by a strain that is not susceptible to antibiotics, phage therapy may be a viable treatment option. Additionally, in cases where a personalized treatment approach is needed, such as in chronic infections or infections with multiple bacterial strains, phage therapy may be more effective than antibiotics.
Are phages more effective than antibiotics?
Phages and antibiotics are both used to treat bacterial infections, but their effectiveness depends on the specific circumstances of each case.
When it comes to clearing one specific bacteria, phages are often more effective than antibiotics. This is because phages are naturally designed to target and destroy specific types of bacteria, while antibiotics are typically broad-spectrum and may harm beneficial bacteria in the body. For example, if a patient is infected with a strain of bacteria that is resistant to commonly used antibiotics, phages may be a viable treatment option.
On the other hand, if a patient is dealing with multiple bacterial infections, antibiotics are typically the preferred option. This is because phages are specific to certain strains of bacteria, and a single phage treatment may not be effective against multiple bacterial species. However, phage cocktails can be used to address this limitation. By mixing together phages that are specific to different bacteria, a phage cocktail can be created that is effective against multiple bacterial infections.
Additionally, the mode of administration can also play a role in the effectiveness of phages and antibiotics. Antibiotics are typically administered orally or intravenously, while phages can be administered via topical application, injection, or oral consumption. In some cases, such as infections in the gastrointestinal tract, phages may be more effective than antibiotics because they can be targeted specifically to the site of infection.
Phage Fast Facts
- Phages won’t harm any of your cells except for the bacterial cells that they’re meant to kill.
- Phage therapy has fewer side effects than antibiotics.
- On the other hand, most antibiotics have a much wider host range. Some antibiotics can kill a wide range of bacterial species at the same time.
- The human immune system sometimes recognizes phages as “foreigners” and tries to kill them. To prevent this, doctors can give their patients large amounts of phage particles or use carrier molecules such as DendriPep.
Bacteriophages are here to save lives especially in a scenario where AMR is concerned. thanks Raph great article.
I am impressed but there is need for more extensive and intensive evaluation on these phage therapeutics.